Preventing the Next Virus
With an on-going respiratory related pandemic and the upcoming flu season it is imperative that a preventative healthcare strategy is implemented to promote good, bronchial hygiene for your at-risk pulmonary patient so they can be in the best health possible for normal, everyday living now and in the future for when the next virus comes.
The possibility of a “twin-demic” is upon us. Influenza season coinciding with the COVID-19 pandemic is cause for concern as it can have serious implications on health care capacity and mortality.¹ Reducing this worst-case scenario is key, and there is at least one factor that can help – the influenza vaccine. A flu vaccine can help decrease health care system burdens and allow those that need medical care to be able to get it.²
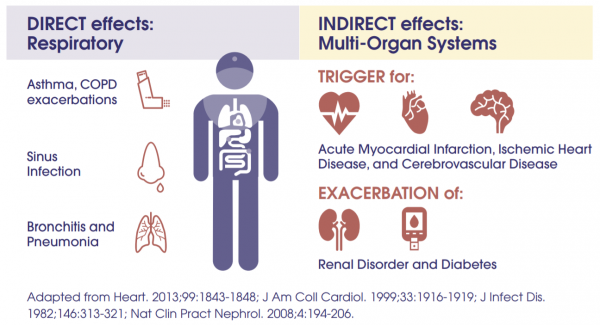
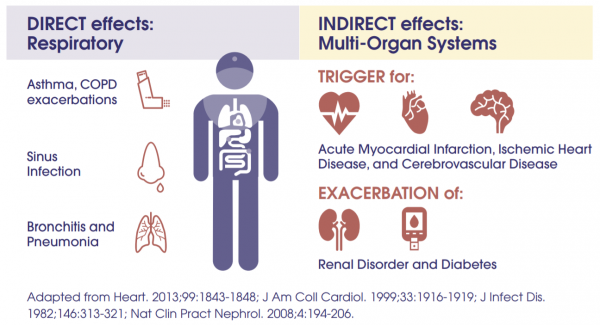
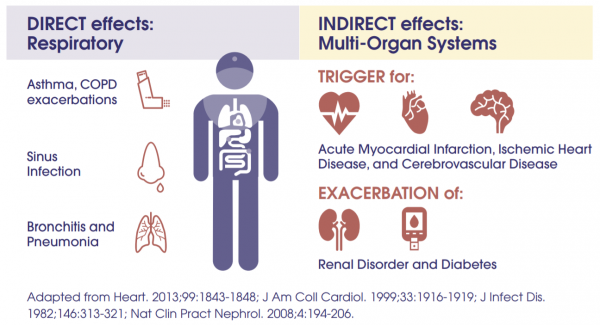
FLU EXACERBATION OF CHRONIC HEALTH CONDITIONS: DIRECT AND INDIRECT EFFECTS
There is heightened importance this year of getting the influenza vaccination to minimize the viral reservoir in the population.³ Low vaccination rates are a missed opportunity for reducing influenza every year but would be especially harmful this year.⁴ According to vaccination rates in the United States from last year (2018 – 2019)⁵
- Only 45% of adults got a flu shot
- 68% of adults over 65-years-old were vaccinated
- Only 48% of young and middle-aged adults with high-risk conditions, like asthma, diabetes, heart disease and COPD were vaccinated
Efforts to increase rates of vaccination against influenza are crucial, especially among older adults who are susceptible to both flu and COVID.⁶ With the Centers for Disease Control hoping to push vaccination rates to 65% overall, this is a tall order to overcome the typical hinderances and the added issues this year due the pandemic, like people wanting to be “safe at home” or reduced access to getting the shot as in years past through work.
An influenza vaccination can help keep people healthy, but what other preventative health measures can be administered for at-risk respiratory patients?
- How can pneumonia be prevented for those at-risk patients that have never had it?
- How can the next pneumonia be prevented for at-risk patients that have had multiple, recurring pneumonias?
The typical first line of treatment for pneumonia is antibiotics. Antibiotics treat the infection. If the patient is treated in the hospital then they also get plenty of fluids, breathing treatments and exercise to help loosen mucus, which can aid in clearing the airways. Depending on the severity of pneumonia, a patient may get oxygen for help in breathing or a bronchoscopy to help clear persistent airway blockages from their lungs. Then when the infection is gone the patient is discharged which is typically within a week. This reactive approach is appropriate and covers all aspects of treating the condition – eliminating the infection and clearing mucus from the airways.
Could a more proactive or preventative approach be beneficial for the at-risk pulmonary patients before they get an infection?
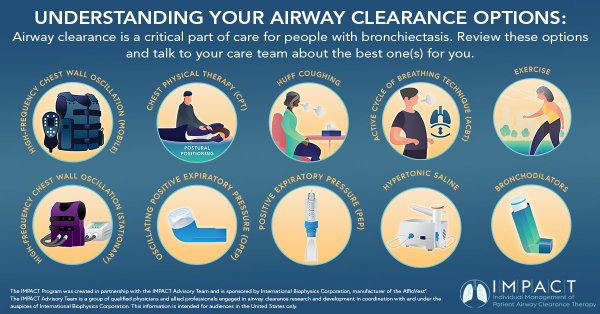
Airway clearance techniques are intended to reduce obstructive secretions, which can include issues like air-flow obstruction, respiratory infection, dyspnea, fatigue, and reduced quality of life.⁷ Patients with a daily, productive cough should be utilizing airway clearance therapy daily to help prevent future infections or hospitalizations.
Effective mucus clearance is essential for lung health, and airway disease is a consistent consequence of poor clearance.⁸ Airway clearance techniques assist with secretion clearance, are widely recommended, and can include both mucus-mobilizing techniques and assisted cough techniques.⁸ Studies recommend that airway clearance techniques be used as the primary method of mobilizing secretions from the middle and small airways to the larger airways. Then, effective coughing can be used to clear secretions from the larger airways, thereby preserving the integrity of the larger airways.⁸
The goal of Airway Clearance Therapy is to provide a preventative treatment option for at-risk pulmonary patients that results in reduced, recurring hospitalizations and better overall health. ⁹’¹⁰
High-frequency chest wall oscillation (HFCWO) airway clearance therapy applies high-frequency vibration to loosen and mobilize mucus. A recent retrospective study showed that patients with COPD and without bronchiectasis showed changes in hospitalization rate as well as self-reported outcomes of respiratory health and ability to clear secretions with the use of high frequency chest wall oscillation.¹¹ According the study, HFCWO vests appeared to reduce COPD exacerbations. After 24 months of wearing the vest, patients achieved a 54.4% reduction in the annualized hospitalization rate for respiratory causes.¹¹
AffloVest Mobile Mechanical HFCWO vest therapy was specifically engineered to mimic the gold standard of manual chest physical therapy, streamline treatment, enhance airway clearance, help mobilize lung secretions, and promote treatment adherence. With no bulky tubes and generators as found in other HFCWO therapies, the AffloVest can be utilized in any postural position (for example laying down, standing, sitting, inclined, reclined, etc.) to help improve secretion mobilization. Recent studies have shown that moving patients into different positions affects ventilation in two different ways. First, a change in body position alters regional ventilation. Second, by increasing the mobility of a patient, oxygen demand increases, resulting in a corresponding increase in minute ventilation and lung volumes. The resultant increase in ventilation allows air to move into obstructed lung units by interdependence and collateral ventilation.⁸
AffloVest is designed to increase therapy adherence through mobility during use, which can provide more consistent therapy compliance and an improved quality of life.

References:
1. Yan, B. et al. How Influenza Vaccination Rate Variation Could Inform Pandemic-Era Vaccination Efforts. J of Gen Internal Med. 2020. August (1-3).
2. Smith, J.R. This might be your most important flu shot ever. CNN Health. September 8, 2020.
3. Solomon, D. et al. Influenza in the COVID-19 Era. JAMA Insights Clinical Review & Education. August 2020.
4. Gostin, L. et al. The Dual Epidemics of COVID-19 and Influenza. JAMA. 2020; 324(4).
5. Jaklevic, M. Flu Vaccination Urged During COVID-19 Pandemic. JAMA Medical News and Perspectives. September 2020; 324(10).
6. Singer, B. COVID-19 and the Next Influenza Season. Science Advances. 2020; 6(31).
7. Andrews, J. et al. Nonpharmacologic Airway Clearance Techniques in Hospitalized Patients: A Systematic Review. Respiratory Care. 2013; 58(12) 2160-2186.
8. McIlwaine, M. et al. Personalizing Airway Clearance in Chronic Lung Disease. European Respiratory Review. 2017; 26.
9. O’Neill, K. et al. Airway Clearance, Mucoactive Therapies and Pulmonary Rehabilitation in Bronchiectasis. Respirology 2019; 24(3):227-237.
10. McShane, P et al. Concise Clinical Review: Non-Cystic Fibrosis Bronchiectasis. Am J Respir Crit Care Med 2013; 188(6):647-656.
11. Hansen, G. et al. Outcomes of High Frequency Chest Wall Oscillation in COPD Patients without Bronchiectasis. CHEST. 2019; 156(4). Supplement. A1170.