Landmarked Pulmonary Clinical Study Published in Respiratory Therapy
HFCWO is a form of Airway Clearance Therapy for bronchial secretion clearance used in the treatment of Cystic Fibrosis, Bronchiectasis, Chronic Obstructive Pulmonary Disease (COPD), neuromuscular diseases and other disorders. It is estimated that over 5 million people in the United States may have Bronchiectasis. Although it has been asserted that vest-induced increased airflow bias in the lungs is one of the modes of action, the actual effect of HCFWO devices on cephalad airflow bias in the lungs during use has not previously been clinically evaluated.
Thomas W. O’Brien, MD, Pulmonologist at Pulmonary Disease Specialists in Kissimmee, Florida and the study’s Principal Investigator, explained its primary purpose.
“It has been claimed that one of the operating principles of HFCWO vests is creating ‘airflow bias’ in the lungs, but valid clinical evidence supporting that claim is lacking. The IRB-Approved Clinical Study aimed to prospectively evaluate lung function scores before, during and after use using different types of HFCWO vests to evaluate the claims of increased vest-induced airflow bias in the lungs.”
The prospective, single-center three-arm study enrolled 32 healthy subjects between February and March 2018. The trial was registered in ClinicalTrials.gov via the Protocol Registration System (PRS), completed under Institutional Review Board (IRB) approval, and published in Respiratory Therapy, the first study of its kind to measure airflow bias during use with HFCWO therapy.
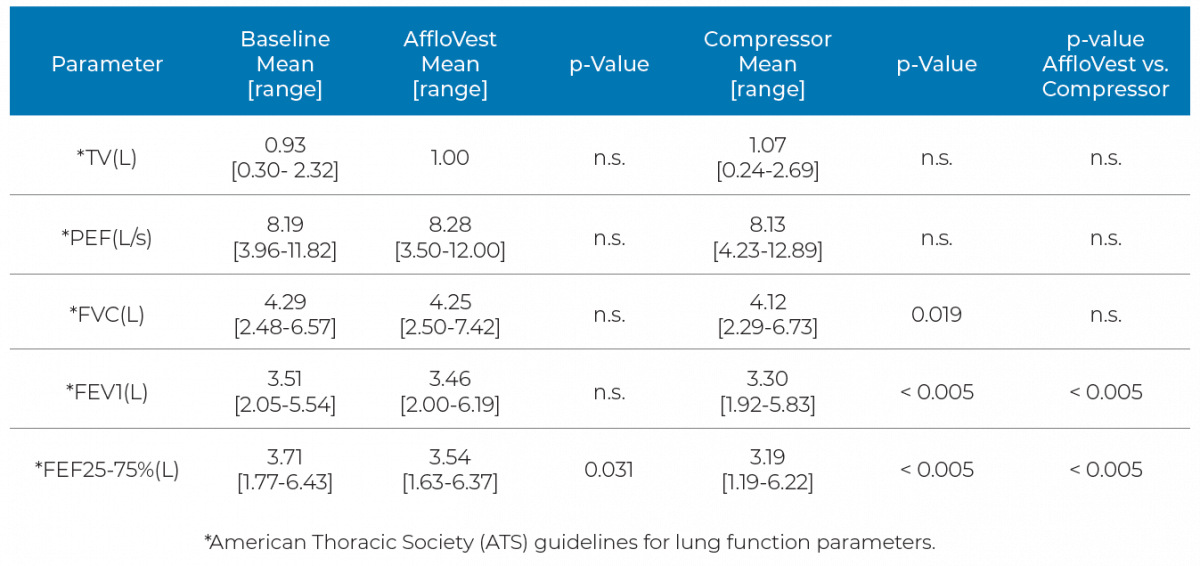
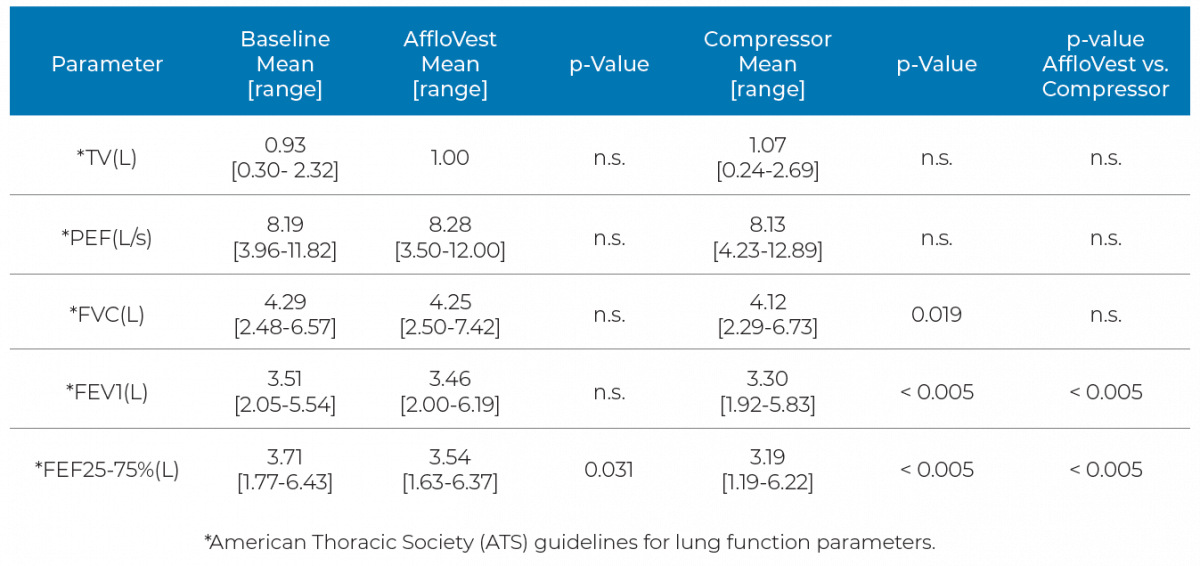
Each subject was assessed according to the American Thoracic Society’s (ATS) guidelines for baseline lung function parameters. Included in these parameters are Forced Vital Capacity (FVC), Forced Expiratory Volume (FEV1), Peak Expiratory Flow (PEF), Tidal Volume (TV) and Forced Expiratory Flow (FEF25%-75%). Each subject was fitted with two different types of HFCWO vests. One type was International Biophysics’ AffloVest® mechanical oscillator-based device, and the other type was one of three compressor-based “air bladder” oscillatory devices (The Vest®, SmartVest®, inCourage®). Lung function tests were then performed on each subject, comparing each subject’s baseline pulmonary lung function values without a vest to the values observed during and after use of an HFCWO vest. Continued O’Brien,
“Vibratory action through the chest wall helps to loosen secretions, much like manual Chest Physical Therapy (CPT). This study was designed to investigate the effects of the application of mechanical oscillatory and compressor-based HFCWO vests during use on standard spirometry parameters. The results are very interesting and clinically relevant.”
The study also found for the first time that the application of compressor-based HFCWO vests led to a significant decrease in FVC, FEV1 and FEF25-75% from baseline during use. In addition, the standard spirometry measurements collected in this study show no increase in PEF in any of the HFCWO vest groups and thus do not support the concept of HFCWO vest-induced cephalad airflow bias in the lungs as an operating principle of HFCWO vest therapy. Although both groups showed a decline in FEF25-75%, the compressor style group decrease in FEF25-75% was 3 times that of the AffloVest®. Lung function measurements returned to baseline after discontinuation of use for both types of HFCWO devices.
David Shockley, International Biophysics’ President and CEO, concluded:
“This clinical study challenges the long-held belief that HFCWO vest-induced cephalad airflow bias correlates to effective airway clearance therapy. Manual Chest Physical Therapy (CPT) has always been considered the gold standard in mobilizing and clearing lung secretions. We engineered and developed the AffloVest to mimic hand CPT using our patented Direct Dynamic Oscillation™ technology that also provides the benefit of mobility and portability during use for the user.”
“We found the results very interesting and clinically relevant.”
Principal Investigator, Thomas W. O’Brien, MD, Pulmonologist at Pulmonary Disease Specialists in Kissimmee, Florida.
No Evidence of Increased Cephalad Airflow Bias in the Lungs During Use
None of the vest groups showed statistically significant increased airflow in the lungs. This does not support increased cephalad airflow bias in the lungs as a mode of action for HFCWO during use.
Reduced FVC/FEV1 Shown in Compressor Style Vest Group
A statistically significant decline of FVC and FEV1 from baseline during use was experienced with compressor style vests, while AffloVest did not.
Reduced FEF25-75%
Compressor style vests showed a decline of 14% during use, 3X more than the AffloVest’s decline in FEF25-75% during use.
Study Results
In this study, the data show for the first time that compressor-based HFCWO vests significantly decreased FVC, FEV1 and FEF25-75% from baseline. Although both groups showed a decline in FEF25-75%, the compressor style group decrease in FEF25-75% of 14%, was 3 times that of the AffloVest of 4.6%. There was no effect on TV or PEF measurements. This study has been published in Respiratory Therapy. An abstract of the study will be published in Pediatric Pulmonology.

References
1. Warwick WJ, Hansen LG. The Long-Term Effect of High-Frequency Chest Compression Therapy on Pulmonary Complications of Cystic Fibrosis. Pediatric Pulmonology 1991;11:265–71.
2. Chakravorty I, Chahal K, Austin G. A pilot study of the impact of high-frequency chest wall oscillation in chronic obstructive pulmonary disease patients with mucus hypersecretion. Int J Chron Obstruct Pulmon Dis 2011;6:693-9.
3.Hansen G, Daignault S, Stiglich J, et al. Registry Outcomes for HFCWO Vest Therapy in Adult Patients with Bronchiectasis. Am J Respir Crit Care Med. 2016;193:A2307
4. Hansen LG, Warwick WJ, Hansen KL, et al. Mucus Transport Mechanisms in Relation to the Effect of High Frequency Chest Compression (HFCC) on Mucus Clearance. Pediatric Pulmonology 1994;17:113–8.
5. Hardy KA, Anderson BD. Noninvasive clearance of airway secretions. Respir Care Clin N Am 1996;2:323-45.
6. Culver BH, Graham BL, Coates AL, et al. Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am J Respir Crit Care Med 2017;196:1463-72.
7. Osman LP, Roughton M, Hodson ME, et al. Short-term comparative study of high frequency chest wall oscillation and European airway clearance techniques in patients with cystic fibrosis. Thorax 2010;65:196-200.
8. Freitag L, Long WM, Kim CS, et al. Removal of excessive bronchial secretions by asymmetric high-frequency oscillations. J Appl Physiol 1989;67:614-9.
9. King M, Zidulka A, Phillips DM, et al. Tracheal mucus clearance in high-frequency oscillation: effect of peak flow rate bias. Eur Respir J 1990;3:6-13.
10. Fink JB. Forced expiratory technique, directed cough, and autogenic drainage. Respir Care 2007;52:1210-21.