Reimbursement Coverage for your AffloVest
Read More
Conducted by: Madeline Vollers BS, Michael Cooper RT, Chicago, IL
High frequency chest wall oscillation (HFCWO) vest therapy is a cornerstone technique in managing cystic fibrosis. The AffloVest is the first fully mobile during use and portable HFCWO vest that facilitates airway clearance by incorporating eight oscillating motors to create eight individual pressure waves that target the lobes of the lungs, much like manual Chest Physical Therapy (CPT)—in order to help effectively mobilize mucus.
In cystic fibrosis, thick and sticky mucus accumulates in organs that include the lungs, making it difficult for patients to breathe. This buildup also increases the chances of bacterial infections, and persistent inflammation can further damage the lungs. High-frequency chest wall oscillation (HFCWO) airway clearance vests, like the AffloVest, are considered the standard of care in chest physical therapy to clear mucus buildup. They work to help loosen the mucus, so that it can be coughed up and removed.
Participants are two 17-year-old females with Cystic Fibrosis. Pulmonary function tests, cough peak flow measurements, and a five question questionnaire were completed bimonthly for three months. Baseline was recorded prior to the patient transition to the AffloVest as the primary airway clearance therapy. Participants were instructed to use the AffloVest daily as part of the patient’s daily regimen.
The study measured FEV1, CPF, and RV. FEV1 is the forced expiratory pressure in the first second, measuring the volume of air that can be forced out in one second after taking a deep breath. CPF is the cough peak flow, a measurement of the muscle strength during cough. RV is the amount of air that remains in the lungs after maximum exhalation. In comparing baseline versus final values, average FEV1 increased 10% or 305 mL, average CPF increased by 33% or 62.5 L/Min, and average RV decreased by 20% or 365 mL.
Equipment used:
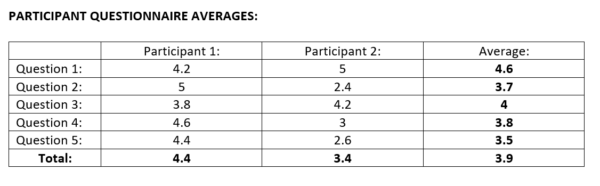
10% IMPROVEMENT IN PREDICTED FEV1
GRAPH A DEPICTS THE GRADUAL IMPROVEMENT OF THE FEV1 FROM 39% TO 49% AFTER USING THE AFFLOVEST.
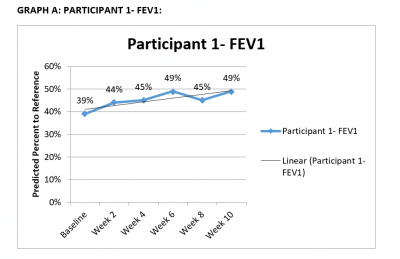
56% IMPROVEMENT IN CPF
GRAPH B DEPICTS THE GRADUAL IMPROVEMENT OF THE CPF FROM 151 L/MIN TO 235 L/MIN AFTER USING THE AFFLOVEST.
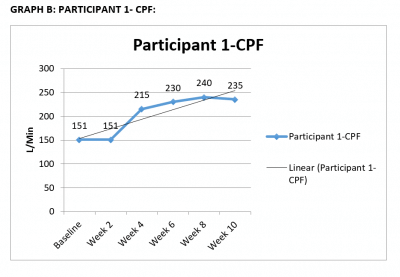
21% (480ML) REDUCTION IN RV
GRAPH C DEPICTS THE REDUCTION IN RV (AIR TRAPPING) FROM 2.33 L TO 1.85 L AFTER USING THE AFFLOVEST.
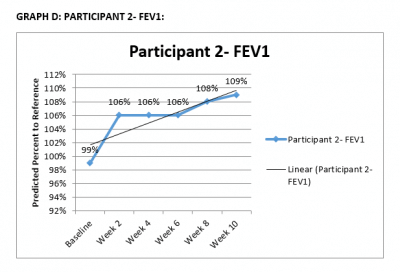
10% IMPROVEMENT IN PREDICTED FEV1
GRAPH D DEPICTS THE GRADUAL IMPROVEMENT OF THE FEV1 FROM 99% TO 109% AFTER USING THE AFFLOVEST.
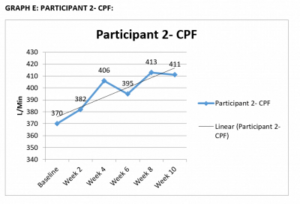
11% IMPROVEMENT IN CPF
GRAPH E DEPICTS THE GRADUAL IMPROVEMENT OF THE CPF FROM 370 L/MIN TO 411 L/MIN AFTER USING THE AFFLOVEST.
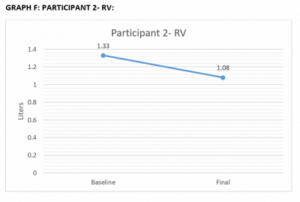
19% (250ML) REDUCTION IN RV
GRAPH F DEPICTS THE REDUCTION IN RV (AIR TRAPPING) FROM 1.33 L TO 1.08 L AFTER USING THE AFFLOVEST.
1.) How well were you able to tolerate the AffloVest this week?
1 2 3 4 5
Very Bad Bad Neutral Good Very Good
2.) How were your energy levels this past week?
1 2 3 4 5
Very Bad Bad Neutral Good Very Good
3.) How often were you coughing this week?
1 2 3 4 5
Rarely Below Average Average Above Average Often
4.) How productive was your cough this week?
1 2 3 4 5
Very Bad Bad Neutral Good Very Good
5.) How was your mucus production this week in comparison to last week?
1 2 3 4 5
Very Bad Bad Neutral Good Very Good
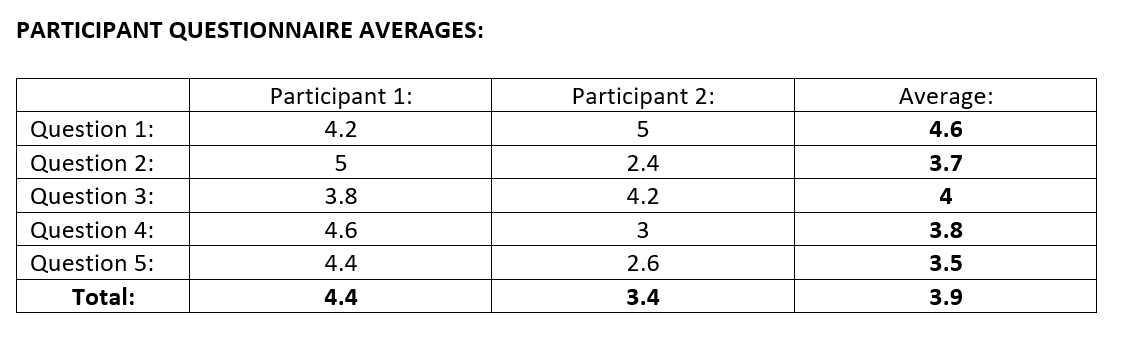
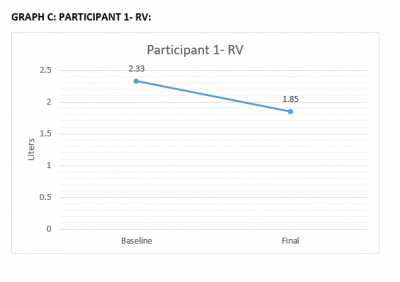
THE PARTICIPANT AVERAGES DEPICTS AN AVERAGE OVERALL RATING OF 3.9 OUT OF 5 (GOOD OR ABOVE AVERAGE) FROM PARTICIPANTS’ QUESTIONNAIRE RESPONSES.
In conclusion, after using the AffloVest for 3 months the test results show continuous improvement in both participants. From baseline to final measurements (3 months) the average FEV1 increased 10% or 305 mL, average CPF increased 33% or 62.5 L/Min, and average RV decreased by 20% or 365 mL.
This was accomplished due to the design and efficiency of the AffloVest. In reducing the RV/air trapping, this allows the participants more functional air, which improves the FEV1. In addition to improving the FEV1, the participant has a greater force of air, producing a stronger cough. This in turn improves CPF values. Both participants liked the mobility and performance of the AffloVest and will continue using this therapy in their daily cystic fibrosis routine.
This study is presented by Independence-U, a non-profit research section of Independence Plus, Inc.
Call us at 1.833.3TACTILE (1-833-382-2845)