Under-diagnosis of Bronchiectasis Hinders Treatment
Read More
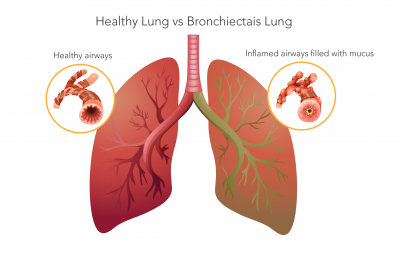
Bronchiectasis (bron-kee-eck-tuh-sis) is a chronic lung condition in which the breathing tubes, also known as airways or bronchi, become abnormally dilated. While there are many causes, damage to the airways by lung infection is the most common. These damaged airways can no longer effectively clear mucus from the lungs.
Over time, the excess mucus creates a breeding ground for bacteria. Here starts a vicious cycle of inflammation and infection, further damaging airways. This can lead to flare-ups of cough, increased mucus production and shortness of breath, called exacerbations. Each exacerbation can make bronchiectasis progressively worse. Therefore, proper treatment to manage symptoms is very important.
Management and treatment of bronchiectasis can include the use of antibiotics to treat lung infections, oral and inhaled medications, and airway clearance therapy such as breathing exercises or HFCWO devices to help clear mucus from the lungs. Patients are often required to do a combination of antibiotic treatments and airway clearance therapies to manage symptoms.
Some treatments and therapies can be complicated and time consuming, leading to issues with adherence to the treatment plan. Treatment adherence has been shown to be low in bronchiectasis and affects important health outcomes including exacerbations. The negative consequences linked to poor treatment adherence in chronic respiratory diseases such as bronchiectasis include higher health care costs, reduced quality of life, increased exacerbations, and the potential for earlier mortality.1
Understanding the importance of utilizing a variety of treatments and therapy options can be difficult for patients. Providing information and education on the various treatment options available may encourage adherence to treatment plans by selecting and adapting a treatment approach that is patient centered. Educating patients with bronchiectasis is recommended, including explanations of the disease, recognition and importance of exacerbations, different treatment approaches and a personalized management plan.2
Bronchiectasis patients should to have easily accessible information about their condition, enabling them to recognize and respond to symptoms appropriately and understand how important adherence to their treatment plan is and how it could potentially alter their prognosis.
Based on answers from a formal questionnaire that was conducted in adult bronchiectasis patients in the Freeman Hospital, the conclusion was drawn that patients with bronchiectasis want more information about their condition. When better informed they feel more confident about management of their condition, with improved symptom awareness, and increased patient satisfaction.4 A recent article written by Katy Hester states that suitable patient information could lead to a level of self-management that results in clinically and biologically important endpoints in bronchiectasis.3
In order to develop patient friendly resources, the underlying needs and issues surrounding information for patients with bronchiectasis must first be fully identified. Educational resources should be available in various settings and formats. Patients should be able to interact with these various resources and access the information as they need it, when they need it, and avoid what they may not need or want to know. Using healthcare experts across the multidisciplinary team, patients and care givers to co-produce high quality information and education resources is an important step towards facilitating self-management advancements, improvements in adherence and consequent physical and psychological health improvements in bronchiectasis.4 Patient education and cooperation with health-care providers to implement treatment plans are key to successful management of bronchiectasis.
References
1. McCullough, Amanda R, Tunney, Michael M, Quittner, Alexandra L, Elborn, J Stuart, Bradley, Judy and Hughes, Carmel M (2014) Treatment adherence and health outcomes in patients with bronchiectasis.BMC Pulmonary Medicine, 14 . p. 107
2. Pasteur MC, Bilton D, Hill AT. British Thoracic Society guideline for non-CF bronchiectasis. 2010;65(Suppl 1)
3. Hester et al. BMC Patient information, education and self-management in bronchiectasis: facilitating improvements to optimize health outcomes. BMC Pulmonary Medicine (2018) 18:80
4. Hester KLM, McAlinden P, De Soyza A. Education and information for patients with bronchiectasis: what do patients want? Eur Respir J. 2011; 38(supplement 35):P3622.
Call us at 1.800.575.1900