COPD Readmissions and Root Cause
22.6%. This is the percentage of COPD patients readmitted within 30-days of hospital discharge.¹ This is a number physicians, clinicians and hospital management know all too well. This number can cause anxiety among healthcare professionals due to the lack of clear consensus and guidelines on how to best predict and prevent readmissions.²
The most recent Kaiser Health News analysis states CMS will fine 2,545 hospitals in fiscal year 2021 for having too many Medicare readmissions within 30 days.³ This is not all for COPD of course. The Medicare readmission penalties cover myocardial infarction, pneumonia, heart failure and COPD among other conditions. The 2,545 hospitals are a reduction of 56% from the prior year which infers that most of the reduction is not related to COPD readmissions.
The cycle of COPD readmissions is not new, but it is a significant problem for 1) physicians and clinicians with many options for treatment but a lack of clear consensus on how to best prevent readmissions 2) patients’ overall mental and physical health, and 3) the whole healthcare system dealing with the costs associated with readmissions even before the Hospital Readmission Reduction Program’s (HRRP) initial release, as part of the Affordable Care Act. In a study last year evaluating the effectiveness of the HRRP the author stated, “5 years after COPD became a target condition for HRRP, there continues to be no single intervention that reliably prevents readmissions in this patient population.”⁴ Therefore treating COPD readmissions is difficult.
Depending on the severity of exacerbation, typical treatments include oxygen therapy, glucocorticosteroids to reduce inflammation, antibiotics, which help a person fight bacterial lung infections, bronchodilators, which can help expand the airways, respiratory stimulants, and respiratory or ventilator support.⁵
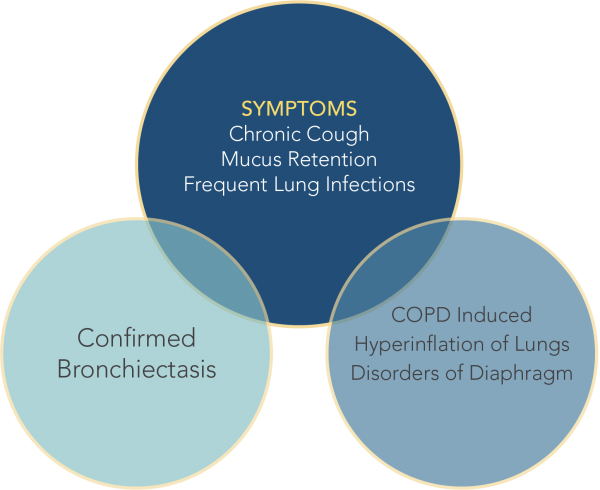
Treating the initial diagnosis of COPD can be difficult as well. With similar or overlapping symptoms across COPD, asthma, and bronchiectasis a proper diagnosis is imperative.⁶ COPD overdiagnosis can delay proper treatment and artificially inflate 30-day readmission rates. A recent study from Cleveland Clinic analyzed their patients that were coded with a COPD hospital discharge in 2018, and they found COPD was over diagnosed and they stressed the caution providers should use when making a COPD diagnosis.⁷
COPD treatment is not all on the healthcare professional. It takes the patient too. Adherence to prescribed medicines and therapies is essential in keeping patients healthy and out of the hospital. Poor adherence to pharmacologic and non-pharmacologic treatment options is one contributing factor to COPD readmissions.⁸
One thing not discussed in the typical treatment options, like treating the infection and opening the airways more, is removing the opportunity for infections to grow. This would be the mucus build up, otherwise known as mucus plugging. Clearing mucus from the lungs can reduce the number of infections and reduce cough and sputum. The addition of identifying the root cause and treating it can provide an opportunity for a change in ideology – going from treatment to prevention.
Dr. Eduardo Mireles-Cabodevila, of the Cleveland Clinic, stated “Before identifying the best possible treatment option, clinicians must first determine the underlying cause of excessive secretions.” in an RT Magazine article on airway clearance options.⁹ This pathway of care can lead to a preventative health strategy for at-risk respiratory patients.
The goal of airway clearance therapy is to provide a preventative treatment option for at-risk pulmonary patients that results in reduced, recurring hospitalizations and better overall health.¹⁰´¹¹
Effective mucus clearance is essential for lung health, and airway disease is a consistent consequence of poor clearance.¹² Airway clearance techniques (ACTs) to assist with secretion clearance are widely recommended and can include both mucus-mobilizing techniques and assisted cough techniques.¹² Studies recommend that ACTs be used as the primary method of mobilizing secretions from the middle and small airways to the larger airways. Then, effective coughing can be used to clear secretions from the larger airways, thereby preserving the integrity of the larger airways.¹²
High-frequency chest wall oscillation (HFCWO) is an airway clearance technique where external chest wall oscillation is applied to the chest using vibrations at variable frequencies and intensities to loosen and mobilize mucus. A recent retrospective study showed that patients with COPD and without bronchiectasis showed changes in hospitalization rate as well as self-reported outcomes of respiratory health and ability to clear secretions with the use of high frequency chest wall oscillation.¹³ According to the study, HFCWO vests designed for treatment of cystic fibrosis, appeared to reduce COPD exacerbations. After 24 months of wearing the vest, patients achieved a 54% reduction in the annualized hospitalization rate for respiratory causes.¹³
The AffloVest Mobile Mechanical HFCWO vest is engineered to mimic the gold standard of airway clearance – manual chest physiotherapy. AffloVest targets all five lobes of the lungs, front and back, with direct dynamic oscillation which allows patients to be fully mobile during use and promotes airway clearance and secretion mobilization. It is the first fully mobile during use HFCWO airway clearance therapy and was designed to deliver mobility and freedom. With no bulky hoses or generators, the AffloVest encourages treatment adherence and compliance by allowing patients to experience an improved quality of life during airway clearance treatments.
COPD or other chronic lung diseases are not covered standalone diagnoses for HFCWO therapy. In these cases, if the patient is experiencing airway clearance issues including daily, productive cough, and well documented failure of other treatment options have been attempted and failed, then a physician can look at other diagnoses that may be occurring due to these chronic lung issues (e.g., disorders of diaphragm, myopathy, etc.)*

*Some insurance requirements vary, please confirm with insurance carrier, Medicare, or Medicaid to make sure all requirements have been met
AffloVest requires a doctor’s prescription for treatment by High Frequency Chest Wall Oscillation (HFCWO). The AffloVest has received the FDA’s 510k clearance for U.S. market availability, and is approved for Medicare, Medicaid, and private health insurance reimbursement under the Healthcare Common Procedure Coding System(HCPCS) code E0483 – High Frequency Chest Wall Oscillation. The AffloVest is also available through the U.S Department of Veterans Affairs/Tricare. Patients must qualify to meet insurance eligibility requirements.
References:
1. Portillo, E. et al. Reducing COPD Readmission Rates: Using a COPD Care Service During Care Transitions. Federal Practitioner. 2018 Nov; 35(11): 30–36.
2. Kong, C. et al. Predicting and Preventing Hospital Readmission for Exacerbations of COPD. European Respiratory Journal Open. 2020
3. Ellison, A. CMS fines 2,545 hospitals for high readmissions: 5 things to know. Becker’s Hospital Review. November 2020.
4. Press, V. et al. Preventing COPD Readmissions Under the Hospital Readmissions Reduction Program How Far Have We Come? CHEST October 2020.
5. Higuera, V. What to know about an exacerbation of COPD. Medical News Today. September 2019.
6. Aksamit, T. et al. Bronchiectasis and Chronic Airway Disease: It Is Not Just About Asthma and COPD. CHEST. October 2018.
7. Rice, R. et al. COPD Overdiagnosis and Its Effect on 30-Day Hospital Readmission Rates. Respiratory Care. January 2021.
8. Mannio, D. et al. Reducing COPD Readmissions: Great Promise but Big Problems. CHEST. May 2015.
9. Airway Clearance: A Range of Treatment Options. RT Magazine. August 2015.
10. O’Neill, K. et al. Airway Clearance, Mucoactive Therapies and Pulmonary Rehabilitation in Bronchiectasis. Respirology. 2019; 24(3):227-237.
11. McShane, P et al. Concise Clinical Review: Non-Cystic Fibrosis Bronchiectasis. Am J Respir Crit Care Med 2013; 188(6):647-656.
12. McIlwaine, M. et al. Personalizing Airway Clearance in Chronic Lung Disease. Eur Respir Rev 2017; 26: 16008.
13. Hansen, G. et al. Outcomes of High Frequency Chest Wall Oscillation (HFCWO) in COPD Patients without Bronchiectasis. CHEST, Volume 156, Issue 4, A1170.