Airway Clearance Therapy for NTM Patients
Read More
The mortality rate from pneumonia in the United States has had limited improvement since antibiotics became widespread more than 50 years ago.¹
Pneumonia is the most common cause of hospital admissions for U.S. adults other than childbirth. About 1 million adults seek care in a hospital for pneumonia yearly and 50,000 die from this disease annually.
Maybe an improved healthcare strategy needs to be established for at-risk patients. Before we get into health care strategies let us review what pneumonia is and who is at-risk.
Pneumonia is a lung infection caused by germs, such as bacteria, viruses, and fungi. There are a number of disease processes that impair ciliary function (removal of microbes up and out of the airways), alter secretion production and mucus consistency, and interfere with the cough reflex. Secretions that accumulate or are stagnant obstruct conducting airways, are conduits for bacterial colonization and infection, evoke inflammatory response, and contribute to airway damage.² The most common type of bacterial pneumonia is called pneumococcal pneumonia and occurs when Streptococcus pneumoniae bacteria spreads from person to person through coughing or close contact. When these bacteria reach the lungs, the lungs’ air sacs (alveoli) can become inflamed and fill up with mucus. This makes breathing more difficult and may reduce oxygen levels in the blood, which can be fatal.³
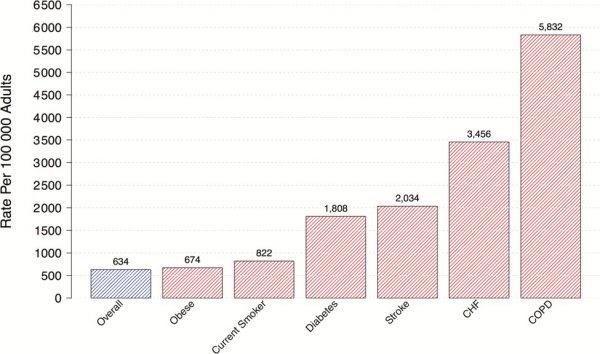
Some people have a higher risk of developing pneumonia, like those with chronic conditions such as COPD and asthma.

Bronchiectasis patients are also at high risk for pneumonia because bronchiectasis causes the airways to be wider than normal. This leads to mucus (or sputum) building up and increasing the patients’ risk of getting lung infections.⁴
It is not a coincidence that people with COPD, asthma and bronchiectasis are at high risk for pneumonia as all these people have compromised lungs with similar symptoms like cough, sputum and dyspnea.⁵
Clin Infect Dis, Volume 65, Issue 11, 1 December 2017, Pages 1806–1812, https://doi.org/10.1093/cid/cix647
Published by Oxford Press. 2017.
A healthcare strategy for pneumonia should be all encompassing as it needs to be proactive and reactive. Antibiotics answers the reactive strategy for bacterial pneumonia, and it works. But what is being done for preventing pneumonia in the first place?
These recommendations are important, but an opportunity is missing from this list — preventing the precursor of infection – which is to clear the mucus build up in the lungs.
Airway clearance techniques are intended to reduce obstructive secretions, which can include issues like air-flow obstruction, respiratory infection, dyspnea, fatigue, and reduced quality of life.⁶ Effective mucus clearance is essential for lung health, and airway disease is a consistent consequence of poor clearance.⁷ Studies recommend that airway clearance techniques be used as the primary method of mobilizing secretions from the middle and small airways to the larger airways. Then, effective coughing can be used to clear secretions from the larger airways, thereby preserving the integrity of the larger airways.⁷
Airway clearance therapy can help keep airways clear which reduces the build-up of lung infections that can result in:
High-frequency chest wall oscillation (HFCWO) airway clearance therapy applies high-frequency vibration to loosen and mobilize mucus. A recent retrospective study showed that patients with COPD and without bronchiectasis showed changes in hospitalization rate as well as self-reported outcomes of respiratory health and ability to clear secretions with the use of high frequency chest wall oscillation.⁸ According the study, HFCWO vests appeared to reduce COPD exacerbations. After 24 months of wearing the vest, patients achieved a 54.4% reduction in the annualized hospitalization rate for respiratory causes.⁸

AffloVest® Mobile Mechanical HFCWO vest therapy was specifically engineered to mimic the gold standard of manual chest physical therapy (CPT). The AffloVest is the first fully mobile, during use, and portable HFCWO vest that facilitates airway clearance by incorporating eight oscillating motors to create eight individual pressure waves that target the lobes of the lungs, much like manual CPT, in order to help effectively loosen, thin and mobilize mucus.
Now is the time to promote good bronchial hygiene for at-risk pulmonary patients with the addition of non-pharmacologic airway clearance therapy, like high frequency chest wall oscillation, to keep at-risk pulmonary patients out of the hospital and provide better overall health. ⁹’¹⁰
References:
1. Top 20 Pneumonia Facts-2019. American Thoracic Society. https://www.thoracic.org/patients/patient-resources/resources/top-pneumonia-facts.pdf
2. Volsko, T. Airway Clearance Therapy: Finding the Evidence. Respiratory Care. 2013; 58(10):1669-78.
3. The Connection Between Pneumonia and Lung Disease. Each Breathe Blog. American Lung Association. November 2018. https://www.lung.org/blog/pneumonia-and-lung-disease.
4. European Lung Foundation. Bronchiectasis. Breathe. 2018 Mar; 14(1): 73–80.
5. Miguel Angel Martinez-Garcia, MA, et al. Bronchiectasis and Chronic Airway Disease: It Is Not Just About Asthma and COPD. Chest Volume 154, Issue 4, Pages 737–739.
6. Andrews, J. et al. Nonpharmacologic Airway Clearance Techniques in Hospitalized Patients: A Systematic Review. Respiratory Care. 2013; 58(12) 2160-2186.
7. McIlwaine, M. et al. Personalizing Airway Clearance in Chronic Lung Disease. European Respiratory Review. 2017; 26.
8. Hansen, G. et al. Outcomes of High Frequency Chest Wall Oscillation in COPD Patients without Bronchiectasis. CHEST. 2019; 156(4). Supplement. A1170.
9. O’Neill, K. et al. Airway Clearance, Mucoactive Therapies and Pulmonary Rehabilitation in Bronchiectasis. Respirology 2019; 24(3):227-237.
10. McShane, P et al. Concise Clinical Review: Non-Cystic Fibrosis Bronchiectasis. Am J Respir Crit Care Med 2013; 188(6):647-656.
Call us at 1.833.3TACTILE (1-833-382-2845)