Minorities with Cystic Fibrosis
Read More
Cystic fibrosis (CF) is an inherited genetic disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, causing the CFTR protein to malfunction. CF affects many systems in the body, but mainly the lungs.1 The progressiveness of the condition leads to loss of lung function through mucus plugging, air trapping and increased lung bacterial infections. CF causes dyspnea – labored breathing — and limits the amount of exercise people with the disorder can tolerate. The pace of this lung disease leads to a low ability to exercise and physical inactivity, which in turn affects health and health-related quality of life.1
However, research and studies have shown that regular physical activity and exercise can provide multiple benefits for people with CF. These benefits go beyond improved lung function, staying fit and physically active. It can also help strengthen bones, manage diabetes and heart disease and improve mental health and quality of life.1 Research findings have extended the understanding of the important role of exercise testing, the physiologic responses to exercise in CF, and of the effects of regular exercise as part of the care continuum for these patients.2
Physical exercise can be defined as participation in a program of regular physical activity designed to improve physical performance, cardiovascular function, muscle strength or any combination of these three.2 There are two different types of physical exercise training: aerobic training or anaerobic training. However, none can be considered purely ‘aerobic’ or ‘anaerobic’ with respect to energy supply. Aerobic training usually involves periods of continuous training (e.g. cycling or running) for a length of time at a target intensity below the anaerobic threshold. Anaerobic training involves training (e.g. weight or resistance training or sprinting) at a high intensity for a short duration above the anaerobic threshold.2
Physical exercise has multiple beneficial effects. It contributes to the alleviation of dyspnea and improves exercise tolerance in people with CF.3 Exercise may facilitate a cough reflex, helping clear mucus from the lungs, allowing for easier breathing. The increased exercise-induced airflows, and related mechanical stress, result in greater ease of coughing up mucus and reduction in mucus viscosity and elasticity, providing benefits like that of traditional airway clearance techniques.3
Physical exercise can improve pulmonary function by improving mucus clearance through a combination of hyperventilation, mechanical vibration, coughing and changes in sputum flow leading to facilitated and increased sputum expectoration.4 The observation that exercise stimulated coughing and increased mucus expectoration in CF patients has led to various studies exploring the use of exercise as a complementary form of airway clearance therapy.2
A 3-year program of exercise therapy shows a decrease in the rate of decline in pulmonary function for a group of mildly to moderately impaired patients with CF. Pulmonary function declined more slowly in the exercise group than in the control group, suggesting a benefit for patients with CF participating in regular aerobic exercise.5 Consistent compliance with a home exercise program and a self-reported positive attitude toward exercise provided further evidence of the feasibility and value of including an aerobic exercise program in the conventional treatment regimen of patients.5
Another study shows a significant association between aerobic fitness and reduced mortality in a large population of patients with cystic fibrosis. The results of this study indicates a notable association between aerobic fitness and stable lung function at eight years among patients with cystic fibrosis.6 Increased fitness, as measured by peak VO₂, is associated with a slower decline in lung function further supporting the use of regular exercise testing to monitor fitness and disease status.2

Being physically active will not just make people with CF feel better, it can improve their quality of life. A significant improvement in health-related quality of life, according to the Quality of Well-being Scale, was observed in the aerobic exercise group compared to the non-physical training group at 1 month after hospital discharge.7
“If you have CF and you’re not working out or doing things that are healthy for you, I think you’re making a huge mistake because we already have so much going against us. We have to be able to be fit and healthy so we can live a long life,” said James Richardson, a CF patient and a certified personal trainer. “Physical fitness and nutrition add years to your life no matter what. It’s a huge part of my life. It’s my every day. I preach it, I do it myself. I think it’s helped me stay healthy and it’s obviously helped me live the life that I live right now. Fitness and nutrition have helped me stay alive; it’s kept me mentally focused it’s kept me physically able to do things that everyone else does.”
AffloVest is the first fully mobile during use HFCWO therapy designed to provide patients the freedom and mobility to customize and enhance airway clearance therapy, help mobilize lung secretions, and promote treatment adherence for CF patients. The battery-powered AffloVest is designed to increase therapy adherence through mobility. The ability to do airway clearance therapy on the go while performing normal, daily activities may provide more consistent therapy compliance and an improve quality of life. Patient-specific therapy consists of 8 anatomically positioned oscillating motors that create individual pressure waveforms to target all lobes of the lungs, posteriorly and anteriorly, to loosen, thin and mobilize lung secretions, and mimic the gold standard, manual chest PT.
A variety of airway clearance therapies may be combined during use with the AffloVest to help optimize airway clearance. With its unique design and the ability to take full, deep breaths during treatment, nebulizer treatments, postural drainage techniques and physical exercise can be combined with AffloVest therapy with the goal of improving mucus mobilization, lung function and a person’s quality of life.

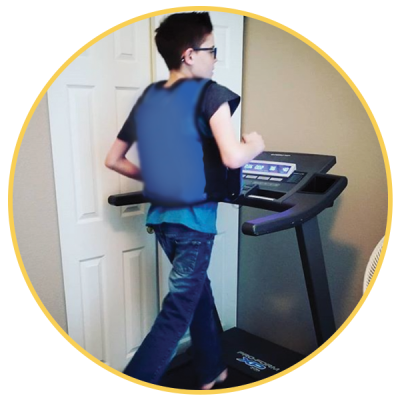
With the mobility that the AffloVest offers, CF patients are able to stay physically active while doing their airway clearance therapy. Because the AffloVest is battery operated and fully mobile during use, people with CF are able to comfortably walk, run or perform HIIT or strength training workouts while doing their AffloVest HFCWO therapy. By complementing exercise with HFCWO airway clearance therapy, patients may cough up more mucus and maintain a better quality of life.
References:
1. CFF Foundation https://www.cff.org/
2. Shephard, Roy J. Aerobic fitness & health. Human Kinetics, 1994.
3. Cerny F. Exercise and Cystic Fibrosis (CF) 2.0. Pediatr Exerc Sci. 2013;25(4):616-623.
4. Dwyer TJ, Zainuldin R, Daviskas E, Bye PT, Alison JA. Effects of treadmill exercise versus Flutter® on respiratory flow and sputum properties in adults with cystic fibrosis: a randomised, controlled, cross-over trial. BMC Pulm Med. 2017;17(1):14.
5. Jane Schneiderman-Walker, MSc, Susan L. Pollock, BPE, Mary Corey, PhD, Donna D. Wilkes, MSc, Gerard J. Canny, MD, Linda Pedder, MD, and J. Joseph Reisman, MD, A randomized controlled trial of a 3-year home exercise program in cystic fibrosis. THE JOURNAL OF PEDIATRICS, VOLUME 136, NUMBER 3 pages 304-310.
6. Orenstein DM, Franklin BA, Doershuk CF, Hellerstein HK, Germann KJ, Horowitz JG, et al. Exercise conditioning and cardiopulmonary fitness in cystic fibrosis. Chest 1981; 80:392-8.
7. Selvadurai HC, Blimkie CJ, Meyers N, Mellis CM, Cooper PJ, Van Asperen PP. Randomized controlled study of in-hospital exercise training programs in children with cystic fibrosis. Pediatr Pulmonol. 2002;33(3):194-200.
Call us at 1.833.3TACTILE (1-833-382-2845)